Despite federal uncertainty, docs embrace 3-D mammography
Published 12:00 am Thursday, January 28, 2016
- Despite federal uncertainty, docs embrace 3-D mammography
Before September 2014, there were no 3-D mammography machines in Bend. A mere 16 months later, they’re the only such machines in town.
The new technology, also called tomosynthesis, produces images that provide a more precise window inside the breast than conventional 2-D mammography, and some research has shown it catches cancers earlier and reduces the number of callbacks for abnormalities that turn out to be benign. Since the federal government approved the first tomosynthesis machine in 2011, the technology has been quickly replacing its predecessors at clinics nationwide.
And yet, the leading federal task force that writes recommendations for clinical services said this month there is not enough evidence to say the risks of tomosynthesis outweigh the benefits. Radiologists across the country and locally say they’re miffed.
“With regard to 3-D mammography, the task force is actually wrong and I disagree with them,” said Dr. Jamie Ockner, a radiologist who interprets images for the Bend Memorial Clinic.
Bend goes 3-D
Far and away the most hotly debated recommendation in the U.S. Preventive Services Task Force’s breast cancer screening statement was that women wait until age 50 to get mammograms. Once they turn 50, the task force says to get the screenings every two years. Countless radiologists, including organizations such as the American College of Radiology, dispute that recommendation, arguing women should begin the screening when they turn 40.
Meanwhile, the tomosynthesis piece created its own — albeit quieter — uproar as countless clinics in the U.S. have already gone full speed ahead with the technology.
BMC was the first provider in Central Oregon to install its one tomosynthesis machine in 2014. The region’s other mammography provider, Cascade Medical Imaging, switched out its 2-D machines for 3-D in February 2015 and now has three tomosynthesis machines in its Bend office and one in its Redmond office. Cascade Medical Imaging, a joint venture between Central Oregon Radiology Associates and St. Charles Health System, provides mammography for patients in Bend, Redmond, Madras and Prineville.
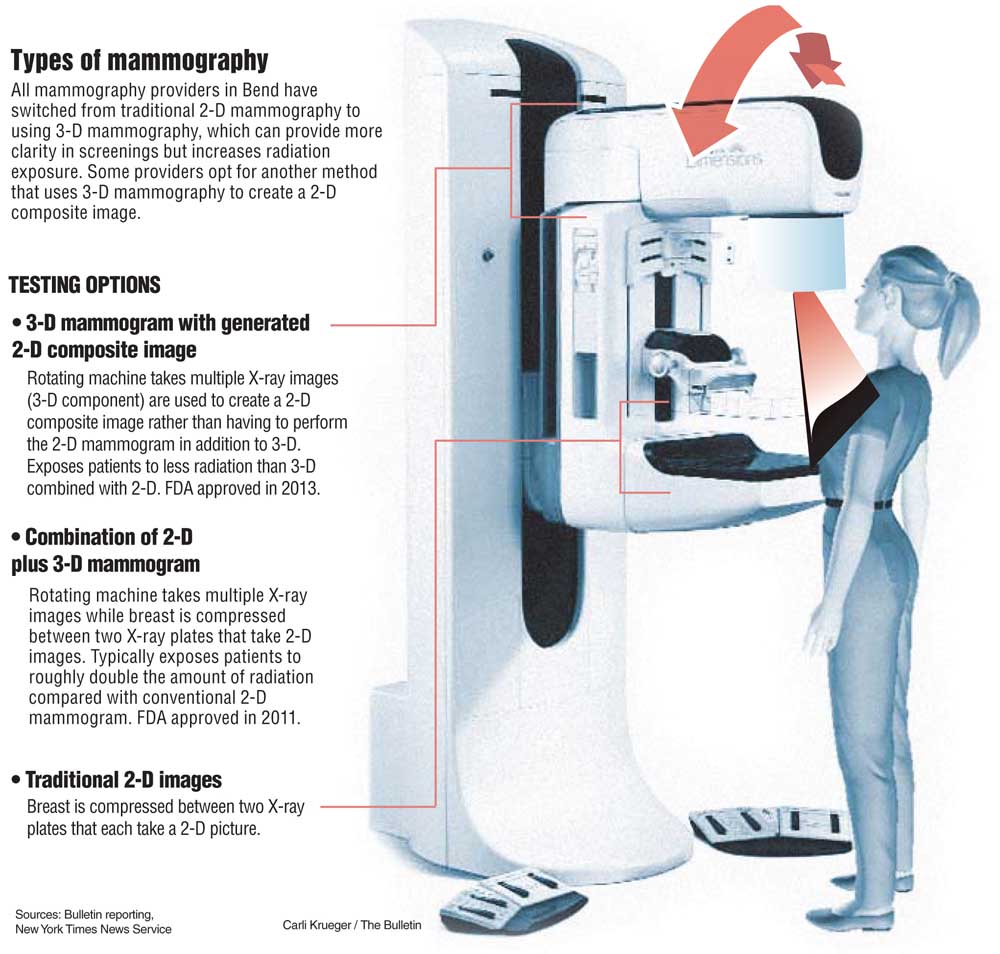
The novel component of tomosynthesis is an arm that rotates in arc motion above the breast, allowing photos to be taken from several angles. These machines still include the longstanding 2-D component: two plates that compress the breast during the screening.
Both 2-D and 3-D mammography rely on X-rays to generate images, which expose patients to radiation. The longstanding drawback of tomosynthesis has been that it exposes patients to a double helping of radiation compared with 2-D alone: that which is emitted during the 2-D scan plus the 3-D scan. Radiologists say the doubled dose is still below the U.S. Food and Drug Administration’s radiation exposure limit for mammograms.
Less radiation with c-view
In 2013, the FDA approved the use of a new tomosynthesis technique that brings its radiation dose roughly back to that of a 2-D scan. Doctors can do this by combining the 3-D images together to create 2-D composite — or c-view — images, negating the need to perform the 2-D exams.
Dr. Cloe Shelton, a radiologist with CORA and Cascade Medical Imaging, said her office now performs 3-D scans plus c-views during all initial screening exams. If abnormalities are found during the screening exam, patients are referred back for what’s called a diagnostic mammogram. For those, patients are still getting the 2-D plus 3-D scans, she said.
BMC is also using 3-D scans plus c-views for mammography screenings in order to limit patients’ radiation exposure, said Ockner, whose main practice is Medford Radiology Associates.
When it comes to diagnostic exams, however, BMC tries to use ultrasound, a technique that uses sound waves to produce images and does not expose patients to radiation. In certain cases, Ockner said BMC will use either a 2-D or a 3-D scan for the diagnostic exam, but not both.
Whether doctors choose to use c-view images and lower patients’ radiation exposure depends largely on their level of comfort with tomosynthesis.
Dr. Debra Monticciolo, chair of the American College of Radiology’s commission on breast cancer, said she still prefers to use both 2-D and 3-D scans instead of c-views, which negate the use of 2-D scans. Having been practicing for 30 years, Monticciolo has spent much of her career using 2-D mammography.
CORA’s Shelton, by contrast, is only four years out from her medical training. She thinks that’s part of the reason she has fully embraced 3-D.
“I wanted it to kind of be an all-or-nothing experience so that we’re getting used to the new technology and learning our strengths and weaknesses with it and not falling back onto the standard 2-D view and to really maximize the benefit of the 3-D,” she said.
Ockner said he, too, feels comfortable using c-view instead of the 2-D scans.
“It’s sort of like ripping off a Band-Aid to get rid of that comfort blanket,” he said. “We did it and it’s worked out well.”
Many people are concerned the new task force recommendations will change whether insurers cover mammograms in certain situations. The Affordable Care Act requires insurers cover any preventive services the task force deems necessary with an “A” or “B” grade, the highest possible. The tomosynthesis statement has an “I” rating.
When providers bill insurers for tomosynthesis, they bill for the conventional 2-D mammogram with the tomosynthesis as an additional charge on top of that. Many prominent insurers, however, don’t cover the 3-D component, including Moda Health, Regence Blue Cross Blue Shield and UnitedHealthcare.
In those cases, both CORA and BMC said they don’t charge patients for the 3-D component.
Dave Magness, CORA’s vice president of clinical operations, said CORA’s doctors ultimately made the decision not to charge patients for the 3-D scans when they were first installed.
“It was a call they made with their eyes open, knowing that, ‘OK, we may not get paid, but we feel that everybody should have the opportunity to get the 3-D because it’s such a good technology,’” he said.
Task force not impressed
For its statement, the task force relied on a Kaiser Permanente report that reviewed 15 tomosynthesis studies.
While the studies showed the practice reduces recall rates and increases cancer detection rates, the report determined they did not answer the question of whether those benefits improved overall clinical outcomes, such as whether women died from the cancer. The studies also didn’t answer the question of whether there was a benefit to detecting said cancers earlier than conventional 2-D mammography would have.
Meanwhile, the task force expressed concern over the potential harm emitted during tomosynthesis. Even though the FDA approved the use of composite views, which emit less radiation, the task force said few screening centers appear to be using that technique.
The Kaiser analysis included a large study published in the Journal of the American Medical Association last year that examined more than 450,000 mammograms, both 2-D and 2-D plus 3-D combined. The study found 2-D exams alone detected 4.2 cancers per every 1,000 exams and the 2-D plus 3-D detected 5.4 cancers per every 1,000 exams. It also found fewer women were called back in for additional testing.
Ockner was sold on the technique in 2013 at a conference in Seattle hosted by Hologic, the manufacturer that made the first FDA-approved tomosynthesis machine and whose machines are in Central Oregon.
After the conference, he was impressed, and convinced his colleagues at BMC to take the leap to 3-D.
“I came out of that course thinking, ‘Holy cow. It feels like malpractice not to have one of these machines,’” he said. “I know that’s an extreme thing to say, but I was so impressed with it. It was just really unbelievable.”
— Reporter: 541-383-0304,
tbannow@bendbulletin.com